Rethinking urban immunization to reach the urban poor
Outbreaks of Vaccine Preventable Diseases (VPD) are more common in urban slums owing to high population density and continuous influx of a new pool of infective agents with the immigrating population. The lack of social fabric in urban slums often limits interpersonal interaction and information about services. Urban poor are often not able to muster enough confidence to access services even when services are proximal. Working mothers do not get the support required to attend to their child’s health needs when they are occupied in livelihood generation activities.
Evidence suggests that poor uptake of immunization in urban areas is associated with mother’s unawareness about repeat visits to achieve complete immunization rather than overall vaccine awareness. Slum dwellers are unable to demand services owing to weak community organisation and low collective confidence which is known to increase utilisation of health services. Immunization programmes in urban areas can exert significant effects on VPD associated mortality by limiting number of cases, decreasing clustering of cases within households and increasing time lapse between outbreaks.
The urban poor population is most vulnerable and deprived when it comes to accessing health care services like immunization. With low immunization coverage in urban and peri-urban pockets, slums and illegal squatter settlements are at a high-risk for outbreaks of VPDs resulting in high morbidity and mortality among infants, children, adolescents and pregnant women. The management of these situations is both challenging and resource-intensive.
The findings of the National Family Health Survey (NFHS)-5 reflect a marginal deterioration in immunization coverage in urban areas. Proportion of fully immunized children, which was marginally higher in urban areas from national and rural averages as per findings of the NFHS-4 survey showed an inverted pattern in NFHS-5 with proportion in urban areas less than both the national as well as rural average.
Fact file
- India’s urban population increased from 25.5% in 1990 to 34.9% in 2020
- Overall, urban growth is expected to contribute to 73% of the total population increase by 2036
- Full immunization drive among children aged 12-23 months recorded substantial improvement from 62% to 76% at all-India level
- 11 out of 14 States/UTs have more than three-fourth children aged 12-23 months with full immunization and it is highest (90%) for Odisha
Source: National Family Health Survey (NFHS)-5
ITSU’s foray in the realm of urban immunization
ITSU’s urban immunization project was launched in December 2020 for a period of three years with the aim of strengthening the overall urban health system with emphasis on immunization services among vulnerable population residing in these areas. The project was implemented in the two states of Uttar Pradesh and Bihar.
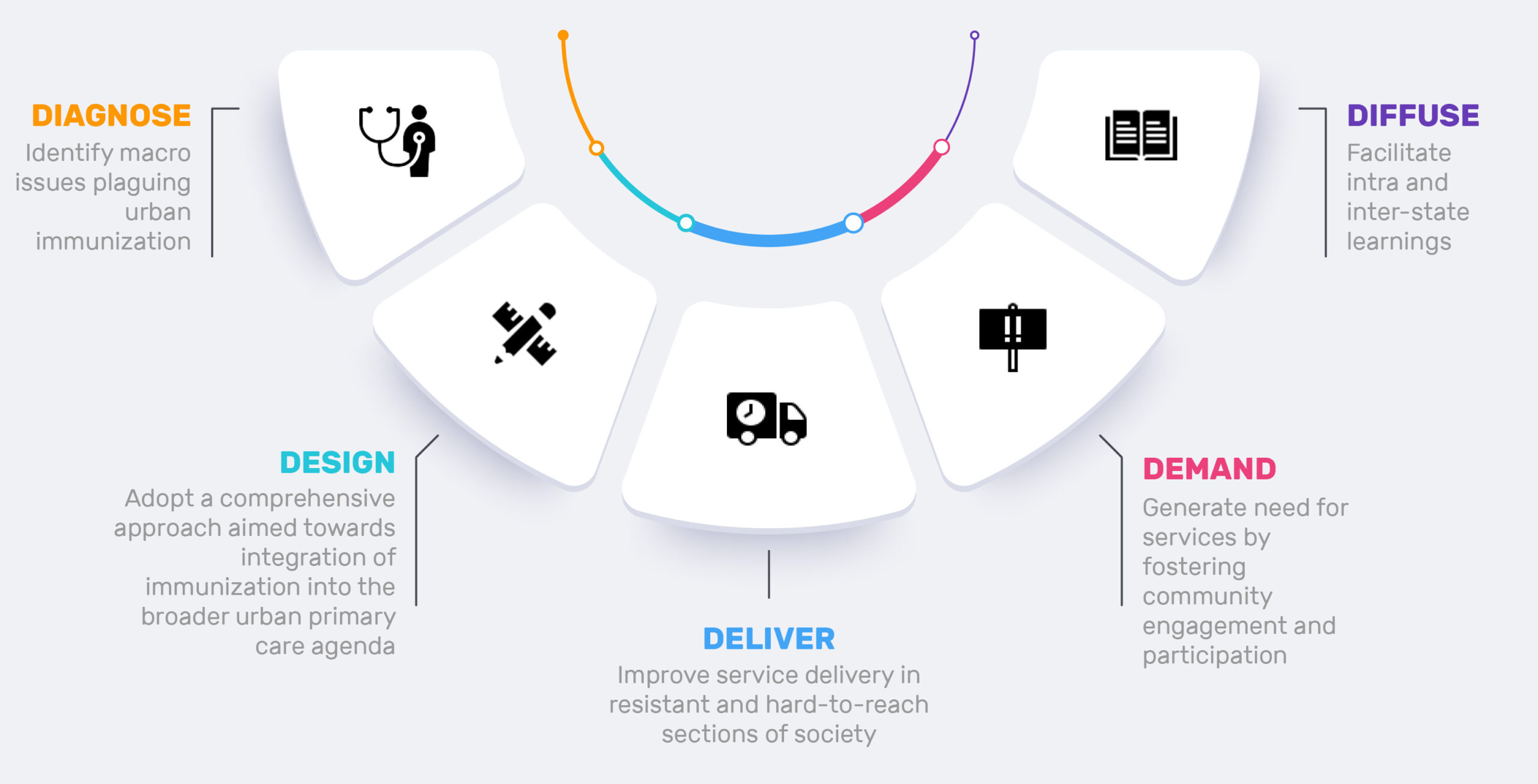
A 5D approach was followed to reach the unreached and to improve vaccination coverage and equity in the project states. The approach includes co-designing new approaches to reach pockets of missed, resistant or under-served communities, and establishes and streamlines review mechanisms and data management systems for local decision making to strengthen immunization systems.
The project also invests in integrating and leveraging RI for urban primary health care systems. The urban immunization issues will be analysed and addressed based on a 5-D cycle to improve outcomes as shown in the below conceptual framework.

5-D Approach followed to strengthen urban immunization in Bihar and UP
The expected outcomes of the urban immunization project include a strengthening of service delivery, raising of demand generation, integrating the project’s goals with other stakeholders and expanding coverage for COVID-19 immunization. By the end of 2023 when the project ends, it is hoped that a clear roadmap would be available to enable the governments of the two project states to scale up across the remaining districts and for other states across the country to adapt and replicate the successful model.


